Trauma-Informed | Evidence-Based | Family-Centered
Prepared by Nurtured by Design, Inc. for NICUs and not for commercial entities.
🚨 This document is a sample protocol intended to serve as a framework for developing or updating your unit’s guidelines for Skin-to-Skin (Kangaroo) Care (SSC). Each NICU should tailor the language, procedures, equipment references, and clinical thresholds based on institutional policies, workflows, staffing models, and patient populations.
This document is provided for informational purposes only and does not constitute medical advice or legal responsibility. Each institution is responsible for reviewing, modifying, and implementing guidelines according to its clinical policies, regulations, and patient safety standards.
I. PURPOSE
To provide a trauma-informed, family-integrated, and evidence-based guideline for implementing Skin-to-Skin (Kangaroo) Care (SSC) in the NICU. This protocol supports safe practices, family empowerment, and performance improvement through consistent data tracking and equitable access.
II. DEFINITION
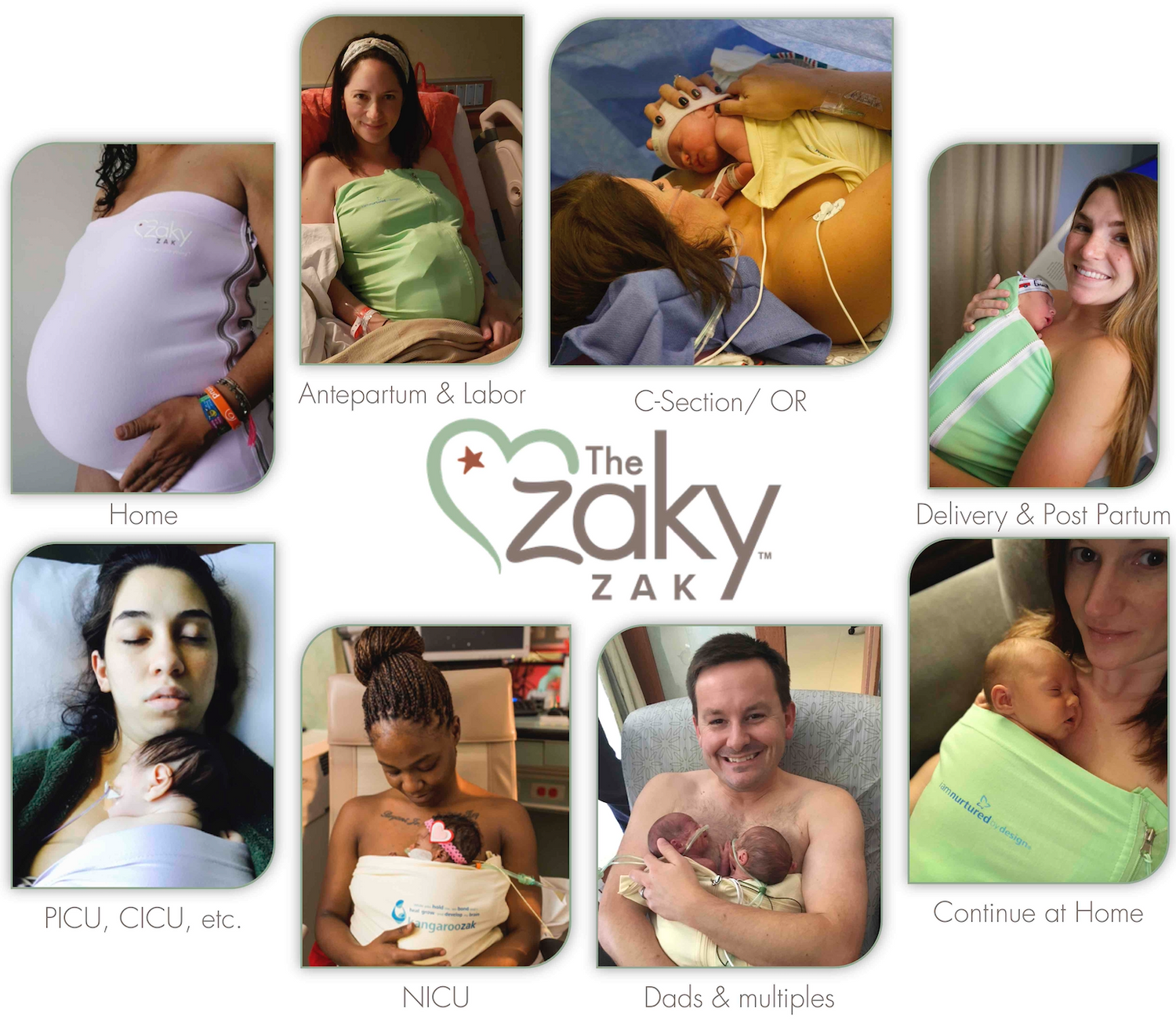
Skin-to-Skin (Kangaroo) Care (SSC): A developmental, healing intervention where a diapered and capped infant is placed directly on the bare chest of a parent or designated caregiver in a vertical or slightly angled position. The dyad is covered with a safety-engineered kangaroo care device to promote safety, warmth, bonding, and physiologic stability.
III. BENEFITS
For Infants:
-
Enhances cardiorespiratory stability
-
Reduces stress, improves sleep and weight gain
-
Supports brain development and feeding readiness
-
Reduces pain, infection, and length of stay
For Caregivers:
-
Builds emotional connection and confidence
-
Reduces stress and trauma symptoms
-
Increases milk production, milk quality, and breastfeeding success
IV. ELIGIBILITY CONSIDERATIONS
A. Eligible Caregivers:
-
Parents (biological, adoptive, foster with documentation) and any person approved by the parents
-
Must have intact skin; no rashes, open wounds, or transmissible infections
-
Free of perfumes, oils, or scented lotions
-
If a caregiver has a medical or physical condition (e.g., poorly controlled seizures, limited mobility, large body habitus), develop a team-based plan for inclusive, safe participation
B. Eligible Infants:
Every infant has the intrinsic right to comfort and connection—NICUs have an obligation to facilitate this safely.
Unless clearly contraindicated temporarily, all medically stable infants should be presumed eligible.
-
Any gestational age or weight
-
On respiratory support (e.g., NCPAP, ventilator)
-
Central lines allowed (PICC, UVC, Broviac)
-
Twins may be held simultaneously if both are stable
C. Temporary Deferral Criteria:
-
Acute instability
-
Escalating ventilator settings or sedation
-
High-intensity phototherapy without biliblanket
-
[Customize for local policy—e.g., ECMO, post-op, complex congenital anomalies]
Eligibility should be reassessed daily with the interdisciplinary team.
V. PREPARATION & EDUCATION
-
Introduce SSC on admission
-
Provide trauma-informed education (verbal, visual, app-based)
-
Encourage but do not pressure; meet families where they are
-
Reinforce WHO guidance of 8–24 hours/day as the goal
-
Normalize SSC for fathers, non-birthing parents, and support persons
"You are not visiting your baby—you are their caregiver."
VI. POSITIONING & TRANSFER
A. Caregiver Setup:
-
Reclined chair, privacy, and gown if needed
-
Bare chest (no bra or shirt under gown)
-
Use safety-engineered SSC device for comfort, support, and access
B. Infant Setup:
-
Diaper placed low to allow chest contact
-
Hat only
-
Lines and tubes secured and untangled
-
Position prone or angled, chest-to-chest
C. Transfer Methods:
-
Standing Transfer (preferred when possible): If caregiver is mobile and trained
-
Sitting Transfer: A clinician transfers the infant to a sitting caregiver.
Emergency equipment must always be within reach. Evaluate if infant shows unresolved signs of distress.
VII. DEVICE USE & SAFETY
-
Use only approved safety-engineered SSC devices (e.g., The Zaky ZAK®)
-
Must support 1–15 lb infants, allow full visibility and airway access
-
Allow quick access for interventions (feeding, emergencies)
-
Never use unapproved upright slings or carriers
-
Follow infection control for cleaning/replacement
-
Document all device use in the EMR
VIII. MONITORING DURING SSC
-
Continuous pulse oximetry (unless otherwise ordered)
-
Temperature before and after SSC
-
Continuous skin probe for infants <1000g
-
For intubated infants: vital signs and pain score at 15 min, then hourly
-
Watch for signs of distress (e.g., desat, apnea, poor perfusion)
IX. INTERDISCIPLINARY COORDINATION
-
Nurses: Lead SSC prep, transfer, monitoring, and charting
-
RTs: Support airway safety and tubing management
-
Music Therapists: Provide soothing rhythm and bonding cues
-
OTs: Optimize infant positioning, coach caregivers
-
PTs: Promote safe postural alignment and motor development
-
Massage Therapists (certified): Support gentle touch techniques
-
Lactation: Integrate SSC with feeding plans
-
Medical Providers: Confirm eligibility, reinforce SSC in rounds
X. DOCUMENTATION & ANALYTICS
A. Clinical Documentation:
-
Time and duration of SSC
-
Name of caregiver
-
Infant’s tolerance and vital signs
-
Method of holding the baby safely (i.e, parent's hands, SSC safety device, etc)
-
Transfer method
-
Any concerns or barriers
-
Parent education provided
B. Quality Tracking (Suggested):
-
% of eligible infants receiving SSC
-
Avg. SSC in the unit - Minutes per baby per day
-
Time to first SSC post-admission
-
Equity indicators (e.g., shift, language, caregiver identity)
-
Staff compliance with documentation
Use tools like The Zaky® App, EMR dashboards, or manual logs to drive improvement.
XI. TRANSITION & CONTINUITY OF CARE
-
Teach SSC safety at home as part of the discharge process
-
Provide printed/home follow-up guidance
-
Encourage continuation of SSC at home until ~3 months corrected age or as tolerated
XII. REVIEW & EDUCATION
-
Annual protocol review or post-incident
-
Staff training should cover:\n - Trauma-informed care
-
Safe transfer/device use
-
Documentation
-
Reducing disparities and unconscious bias
-
XIII. REFERENCES
Prepared by Nurtured by Design, Inc. for NICUs and not for commercial entities.